Fentanyl vs Morphine: Understanding the Differences and Uses
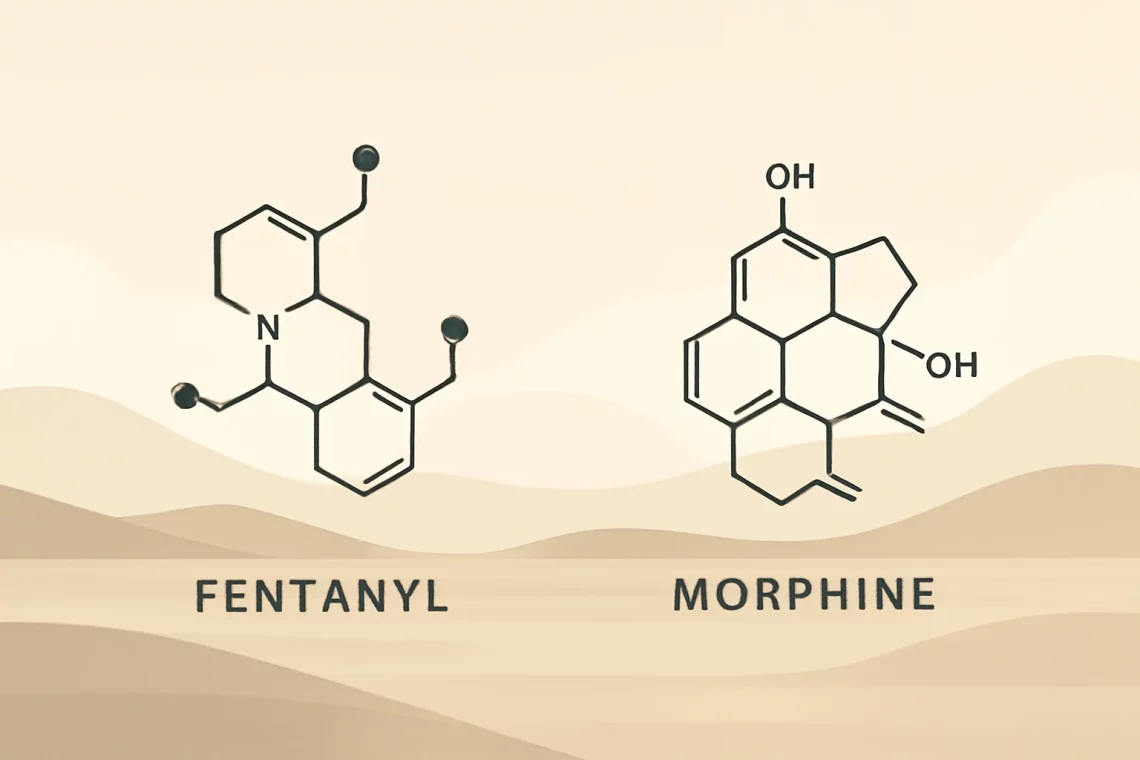
Fentanyl and morphine are two potent medications commonly used in the management of pain. Their effectiveness, however, is accompanied by significant differences in their properties, effects, and potential risks. As healthcare professionals and patients navigate the complex landscape of pain management, understanding these differences is crucial. Fentanyl, a synthetic opioid, is known for its rapid onset and high potency, making it a powerful tool in acute pain scenarios, particularly in surgical settings and for patients with severe chronic pain. Morphine, on the other hand, is a naturally occurring opioid that has been used for centuries to relieve pain. Its well-established efficacy and safety profile make it a go-to choice for many clinicians.
Despite their similarities as opioids, fentanyl and morphine operate through different mechanisms and have varying pharmacokinetics. This leads to distinct clinical applications, advantages, and drawbacks for each medication. With the increasing concern over opioid misuse and addiction, understanding the nuances between these two drugs has never been more critical for both healthcare providers and patients alike. As we delve into the characteristics of fentanyl and morphine, we’ll uncover the implications of their use in pain management and the importance of making informed decisions based on individual patient needs.
Understanding Fentanyl
Fentanyl is a synthetic opioid that is approximately 50 to 100 times more potent than morphine. It was first synthesized in the 1960s and has since become a critical component in pain management, especially in surgical and cancer settings. Fentanyl acts by binding to the body’s opioid receptors, which are located in the brain and spinal cord, effectively blocking the perception of pain. Its rapid onset of action makes it particularly useful in emergency situations where immediate pain relief is required.
One of the unique characteristics of fentanyl is its formulation. It is available in various forms, including patches, lozenges, and injectable solutions. The transdermal patch, for instance, allows for continuous delivery of the medication over several days, providing long-lasting pain relief for patients with chronic pain conditions. This method can be advantageous for those who have difficulty swallowing pills or who require consistent pain management without frequent dosing.
Despite its efficacy, fentanyl also comes with a considerable risk of side effects and potential for misuse. The drug can cause respiratory depression, particularly in individuals who are opioid-naïve or those with certain health conditions. This risk has led to increased scrutiny and regulation surrounding fentanyl prescriptions. The opioid epidemic has highlighted the dangers associated with fentanyl misuse, with many cases of overdose linked to illicitly manufactured fentanyl.
Healthcare providers must carefully assess each patient’s needs and medical history before prescribing fentanyl. Proper education about the drug, its uses, and potential risks is essential for both patients and their families. By fostering an open dialogue, healthcare providers can help patients make informed decisions about their pain management options.
Exploring Morphine
Morphine is often referred to as the gold standard in pain management. Derived from the opium poppy, morphine has been used for centuries and is well-documented in its efficacy and safety. It is primarily used to treat moderate to severe pain and is commonly administered in hospital settings for post-operative pain relief or in palliative care for patients with terminal illnesses.
Like fentanyl, morphine works by binding to opioid receptors in the brain and spinal cord. However, its potency is lower than that of fentanyl, which means that higher doses may be required to achieve the same level of pain relief. Morphine is available in various forms, including oral tablets, liquid formulations, and injectable solutions, allowing for flexibility in patient care.
One of the significant advantages of morphine is its extensive clinical history. Healthcare providers have a wealth of data regarding its effectiveness, safety profile, and potential side effects, which include drowsiness, constipation, and nausea. While these side effects can be managed, they can also lead to complications, particularly in elderly patients or those with pre-existing health issues.
Morphine’s slower onset and longer duration of action compared to fentanyl may make it a more suitable option for patients with chronic pain who require ongoing management. Additionally, the drug is often used in combination with non-opioid pain relievers to enhance its effectiveness and minimize the required opioid dosage.
Despite its long-standing reputation, morphine is not without risks. The potential for addiction and tolerance exists, necessitating careful monitoring and adjustment of dosages. Patients should be educated about the signs of misuse and the importance of adhering to prescribed regimens to mitigate these risks.
Comparing Efficacy and Safety
When comparing fentanyl and morphine, one must consider efficacy, safety, and the context in which each drug is used. Fentanyl’s high potency and rapid action make it an excellent choice for acute pain management, particularly in surgical settings. Its various formulations, such as patches and lozenges, provide flexibility for patients requiring consistent pain control.
Morphine, while less potent, has a more extensive history of use, which contributes to a deeper understanding of its safety and side effects. Its slower onset may be advantageous for patients who do not require immediate pain relief, allowing for a more controlled pain management plan.
Safety is a significant concern with both medications. Fentanyl’s risk of respiratory depression is higher, particularly in opioid-naïve patients, making careful monitoring essential. Conversely, morphine’s side effects, while serious, are typically more predictable, allowing for established protocols for management.
Both medications carry the risk of addiction and require careful patient selection, monitoring, and education. It is crucial for healthcare providers to weigh the benefits and risks of each medication and to engage in shared decision-making with patients. A thorough assessment of the patient’s pain levels, medical history, and potential for substance use disorder will guide the choice of therapy.
Ultimately, the decision between fentanyl and morphine should be individualized, taking into account the specific needs of the patient and the clinical context. By understanding the differences and similarities between these two opioids, healthcare providers can better navigate the complexities of pain management.
Conclusion
In the realm of pain management, fentanyl and morphine serve as essential tools for alleviating suffering. Both opioids demonstrate significant efficacy, yet they differ significantly in potency, safety profiles, and clinical applications. Fentanyl’s rapid onset and high potency make it suitable for acute pain relief, whereas morphine’s established history and predictable side effects lend it to chronic pain management.
As the opioid crisis continues to shape the landscape of pain management, healthcare providers must remain vigilant in their prescribing practices. Educating patients about the risks and benefits of these medications is paramount in promoting safe and effective pain management. With a thorough understanding of fentanyl and morphine, providers can make informed decisions that prioritize patient safety while effectively addressing pain.
It is essential to remember that this article is not a substitute for professional medical advice. For any health-related concerns or questions about pain management, individuals should consult with their healthcare provider.




